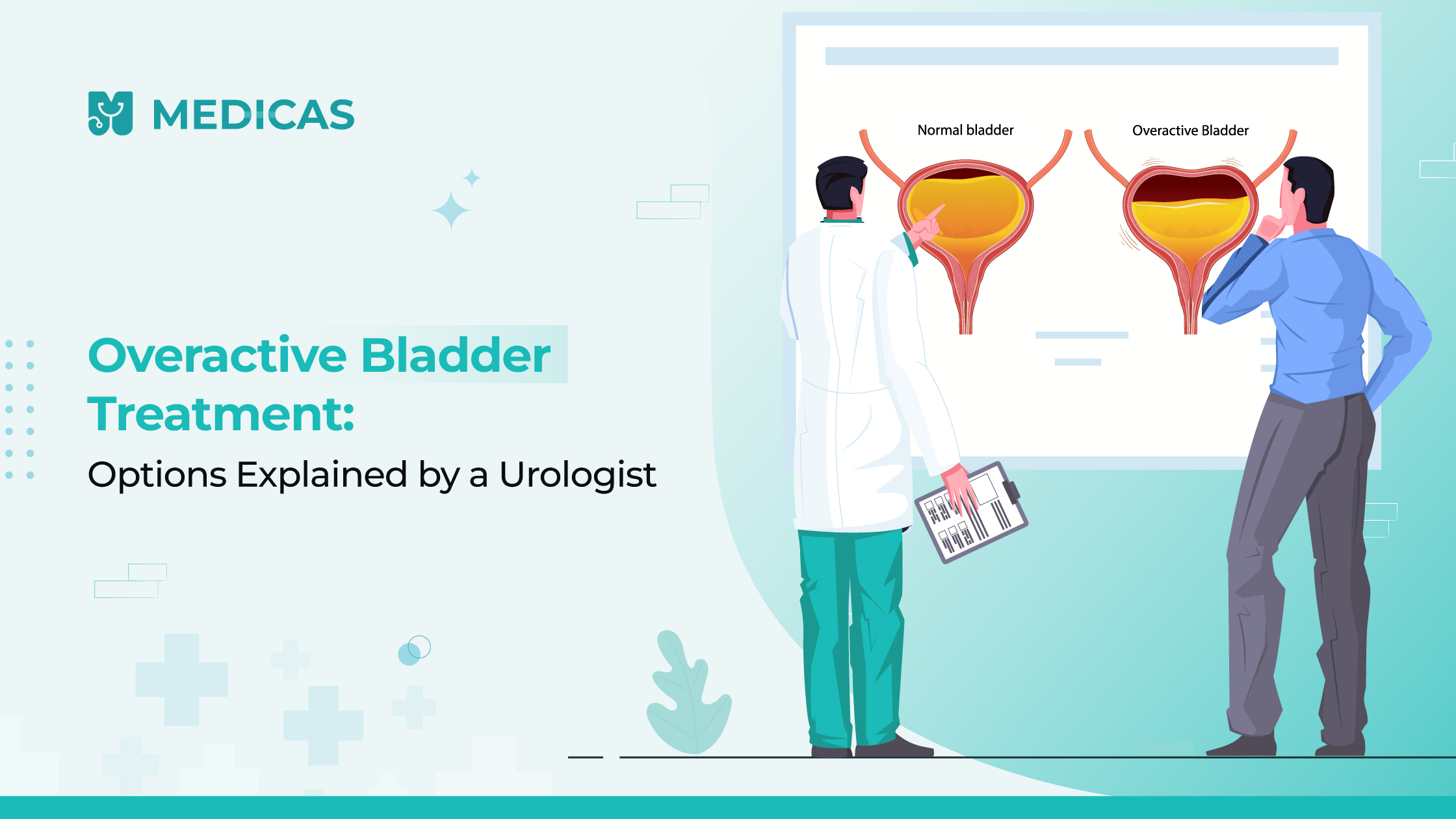
What Is Overactive Bladder (OAB)?
Did you know that overactive bladder affects up to 33 million people? It causes sudden urges to urinate, frequent trips to the bathroom, and sometimes leakage. Understanding overactive bladder treatment begins with recognizing the condition, not just tolerating nuisance symptoms. This guide provides a full-fledged dissection of medical, lifestyle, and even Overactive Bladder Ayurvedic Treatment to make informed decisions.
Definition and Common Symptoms
Overactive Bladder is defined by urgency (with or without leaks), frequent urination (eight-plus times per day), nocturia (waking to pee), and sometimes urinary incontinence. Recognizing these early helps with timely treatment.
Related read: Understanding Urinary Tract Infection
Causes and Risk Factors
- Involuntary bladder muscle contractions happen even when the bladder isn’t full.
- Neurological conditions such as multiple sclerosis, Parkinson’s disease, or stroke, which interfere with signals between the brain and bladder.
- Bladder outlet obstruction (like in men with enlarged prostates) irritates the bladder muscles.
- Hormonal changes during menopause weaken pelvic muscles and impact bladder control.
Related read: Frequent Urination in Summer? Causes, Risks & When to Seek Help
When to See a Doctor for Bladder Issues
- Sudden, intense urges to urinate even when the bladder isn’t full.
- Frequent urination (more than eight times in 24 hours: Waking up multiple times during the night to urinate.
- Urge incontinence: Inability to hold urine once the urge begins.
- Disruption of daily life: Avoiding social activities, work, or travel due to fear of leaks or urgency.
It’s also important to visit your doctor if you’re considering a natural remedy for overactive bladder treatment or Overactive Bladder Ayurvedic Treatment to ensure the safety and compatibility of these remedies with any current conditions or medications.
Suggested read: UTI Symptoms in Women
How Overactive Bladder Is Diagnosed
Medical History Review
- Discussion of symptoms, fluid intake, lifestyle, and any medications being used.
- Questions around when the symptoms started, how often they occur, and whether they affect sleep or daily function.
Bladder Diary
- A 3–7 day log of fluid intake, urination times, volume passed, and urgency episodes.
- Helps identify triggers like caffeine or fluid timing.
Physical Examination
- Includes a pelvic exam (in women) or prostate exam (in men) to assess for muscle weakness, enlargement, or pelvic floor issues.
Urine Tests
- Urinalysis to rule out infection or blood in the urine.
- Culture may be done if infection is suspected.
Ultrasound
- Checks post-void residual (how much urine remains after urination), especially in those with incomplete emptying or dual symptoms (urgency and retention).
Urodynamic Studies
- A more detailed test to measure pressure inside the bladder, urine flow, and how well the bladder fills and empties.
- Often used if initial treatments aren’t effective.
Cystoscopy (if needed)
- A thin tube with a camera is inserted into the bladder to check for stones, tumors, or anatomical abnormalities.
Physical Exams and Bladder Diaries
A pelvic examination can be performed to examine pelvic muscles, prostate (men), or neuropathy. The information provided by a bladder diary that follows fluid, urination, and leakage incidents throughout the duration of a few days is priceless.
Urine Tests, Ultrasounds & Urodynamic Studies
Urinalysis eliminates infections or blood. Ultrasound measures post-void urine. Urodynamic testing tests bladder pressure and bladder capacity, and these are important in assessing dysfunction.
Ruling Out Urinary Tract Infections or Other Issues
UTI is able to mimic the symptoms of OAB; hence, differentiation is done by lab culture. Structural anomalies, bladder stones, or cancer requiring alternative treatment may be discovered by imaging.
Overactive Bladder Treatment Options You Should Know
An individual treatment plan usually begins mildly and graduates to the rate required. It can be treated using behavioral techniques, medications, nerve treatment, natural medications, and some extreme procedures.
Lifestyle and Behavioral Changes
The voiding can be improved through bladder training, timed voiding, reduction of weight, quitting smoking, as well as management of constipation, as they lessen the lower urinary tract symptoms through minimizing bladder irritation and straining of muscles.
Pelvic Floor Exercises (Kegels)
Kegel exercises lead to the strengthening of pelvic muscles, which inhibit bladder contractions. Hold 5 seconds, release, and repeat 10- 15 times in one session. Consistency 2 times a day helps achieve more control.
Medications to Calm Bladder Muscles
Anticholinergics (oxybutynin, tolterodine) or β3 agonists (mirabegron) reduce muscle overactivity. Always discuss side effects like dry mouth or higher blood pressure with your healthcare provider.
Nerve Stimulation Therapies (PTNS, Botox)
PTNS applies mild electrical stimulation to nerve points at the ankle, whereas Botox injection forms a paralysis of overactive muscles of the bladder by blocking nerve signals, which proves highly effective in cases where medications are not functional.
Advanced Treatment: Surgery or Catheter Use
Surgery may rarely be suggested to increase the capacity of the bladder, or a surgeon may use nerve stimulators. Catheterization is reserved for severe cases where retention or incomplete emptying occurs.
Suggested read: What Your Urine Color Says About Your Health
Home Remedies and Daily Habits That Can Help
Often overlooked, simple habits can meaningfully support bladder health and may complement professional overactive bladder treatment regimes, especially for milder cases.
Bladder-Friendly Diet Tips
Limit bladder irritants: caffeine, alcohol, artificial sweeteners, citrus, and spicy foods. Instead, opt for water and hydration-balanced fluids to reduce urgency episodes.
Managing Triggers Like Caffeine and Alcohol
These stimulants can increase urgency and frequency. Try substituting them gradually and monitor response in your bladder diary.
Importance of Hydration Without Overdrinking
Drink to thirst and avoid both under- and over-hydration. Spreading fluid intake evenly throughout the day helps control urgency and reduce nighttime bathroom visits.
When to Visit a Urologist vs. a General Physician
If symptoms are mild and infrequent, start with your GP. But if you experience frequent leaks, recurring UTIs, pain, or incomplete emptying, a urologist’s expertise may be required.
Role of Your GP in Initial Management
GPs can diagnose UTIs, offer first-line behavioral and medication advice, and refer you to a specialist when appropriate.
When Advanced Urological Help Is Needed
Persistent symptoms, medication side effects, catheter dependency, or need for procedures like Botox or neurostimulation warrant a specialist evaluation.
Final Thoughts
Treatment of overactive bladder involves more than just medicines; it is also about learning what makes it happen and what makes it not, then training that behavior and making changes to fit your lifestyle. Guided-based support, pelvic strengthening, bladder awareness, and professional treatment, where necessary, result in a lot of individuals getting control effectively. Be it the natural remedy for overactive bladder treatment, overactive bladder, or the traditional treatment, it is a step in the right direction to better living and better confidence. If you’re facing bladder urgency, don’t wait it out. Book an appointment with a uro-specialist or start with an online consultation to design a treatment plan aligned with your lifestyle and goals.
Frequently Asked Questions (FAQs)
How to fix an overactive bladder?
Treatment of the overactive bladder is done through a coordinated combination of lifestyle choices and pelvic floor training, bladder training, medication, and nerve stimulation therapies in others. With or without medical care, long-term relief can also be achieved through dietary changes and the use of bladder irritant reduction.
What can I drink to stop frequent urination?
Consume drinking water moderately (daily). Do not take caffeine products, especially those that are carbonated, and alcohol. They irritate the bladder. Herbal teas such as chamomile or corn silk tea can be used to reduce the urgency, although you should always be advised by a doctor before applying remedies.
What is the best treatment for an overactive bladder?
The most appropriate treatment is based on the level of severity. It may involve behavioral therapy, Kegel exercises, drugs (such as anticholinergics or 3 agonists), Botox injections, or nerve stimulation. Some individuals may find help in Overactive Bladder Ayurvedic Treatment; however, under the control of a qualified practitioner.
Can general physicians treat OAB, or is a urologist necessary?
The management of OAB at its early stages can be done by general physicians; medications can be prescribed, and some lifestyle changes will be advised. Nevertheless, when the problems are persistent, aggravated, or when the treatment is ineffective, a specialist is to be disabled to assess the situation and provide modern management.
Disclaimer
Medical Advice: The information provided in this blog post is for educational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare professional for personalized guidance regarding your specific medical condition.
Accuracy of Information: While we strive to provide accurate and up-to-date information, the field of medicine and viral fevers is constantly evolving. The content in this blog post may not reflect the most current research or medical guidelines. Therefore, it is advisable to cross-check any information provided with reliable sources or consult a healthcare professional.
Individual Variations: The symptoms, causes, treatment options, and preventive measures discussed in this blog post are general in nature and may not apply to everyone. It is important to remember that each individual’s situation is unique, and personalized medical advice should be sought when making healthcare decisions.
External Links: This blog post may contain links to external websites or resources for additional information. However, we do not endorse or have control over the content of these third-party websites. Accessing these links is done at your own risk, and we are not responsible for any consequences or damages that may arise from visiting these external sources.
Results May Vary: The effectiveness of treatment options or preventive measures mentioned in this blog post may vary from person to person. What works for one individual may not work the same way for another. It is essential to consult with a healthcare professional for personalized advice tailored to your specific needs

Dr. Anuj Arora is a Consultant Urologist and Uro-Oncologist based in Greater Noida and Noida, with over 13 years of medical experience. He completed his MBBS and MS from Maulana Azad Medical College, Delhi, and MCh in Urology from Sri Ramachandra Medical College, Chennai. Dr. Arora has worked with top hospitals including Apollo Spectra and Max Super Speciality Hospital. His areas of expertise include Endourology, Kidney Transplantation, Robotic Urology, and Uro-Oncology. He is a member of USI, UAA, and AUA.